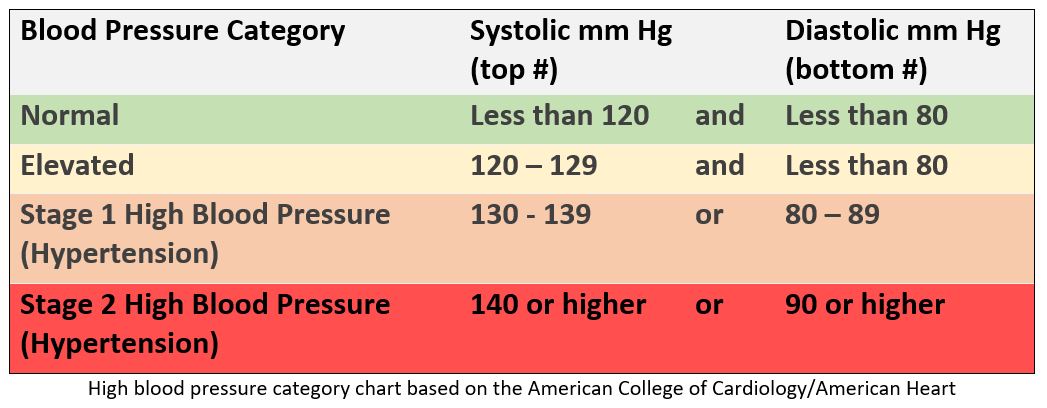
According to 2017 hypertension guidelines from the American College of Cardiology and American Heart Association, the types of blood pressure are defined as:1
- Normal: less than 120 systolic and less than 80 diastolic
- Elevated blood pressure: 120 – 129 systolic and less than 80 diastolic
- Stage 1 hypertension: 130 – 139 systolic or 80 – 89 diastolic
- Stage 2 hypertension: 140 or higher systolic or 90 or higher diastolic
When the numbers for systolic and diastolic pressure fall into different categories, the higher number is used to classify blood pressure.1 For example, a blood pressure of 141/86 mm Hg would be classified as Stage 2 hypertension. These categories help determine when and how to treat high blood pressure.
Studies suggest the risk for heart attack, stroke and other high blood pressure complications begins to increase around 115/75 mm Hg.1-5 The risk continues to increase as blood pressure increases at a rate that about doubles the risk for each 20 mm Hg increase in the systolic pressure and each 10 mm Hg increase in the diastolic pressure. This risk increase was detailed in a 2002 meta-analysis of 61 studies encompassing 958,074 patients and 12.7 million person-years at risk.2 The analysis found 56,000 vascular-related deaths. For people ages 40 to 69 years, a rise of 20 mm Hg systolic blood pressure or 10 mm Hg diastolic more than doubled the risk of death by stroke and doubled the risk of death from ischemic heart disease and other vascular causes. The risks continue to increase with both age and higher blood pressure.
People with high blood pressure often have no signs or symptoms.6 The U.S. Preventive Services Task Force recommends annual screening for adults aged 40 years or older and for those who are at increased risk for high blood pressure. Persons at increased risk include those who have high-normal blood pressure, those who are overweight or obese, and African Americans. Adults aged 18 to 39 years with blood pressure <130/85 mm Hg who do not have other risk factors should be rescreened every three to five years.
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360 (9349): 1903-1913.
- Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383 (9932): 1899-1911.
- Reboussin DM, Allen NB, Griswold ME, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017.
- Wright JT, Jr., Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373 (22): 2103-2116.
- Siu AL. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2015; 163 (10): 778-786.

.png)
